Background
Our understanding of the meniscus has changed radically in the last century. In 1887, Sutton described the meniscus as "the functionless remains of a leg muscle."[1] Not until 1948 did Fairbanks appreciate that "meniscectomy is not wholly innocuous," in his classic report of postmeniscectomy radiographic changes.[2] Research and knowledge of the meniscus has continued. The critical importance of the meniscus of the knee joint is now understood.
Note the contrasting images below.
 Magnetic resonance imaging scan showing a normal meniscus.
Magnetic resonance imaging scan showing a normal meniscus. 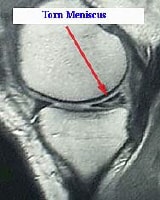 Magnetic resonance imaging scan showing a torn medial meniscus.
Magnetic resonance imaging scan showing a torn medial meniscus. For patient education resources, see the Foot, Ankle, Knee, and Hip Center and Arthritis Center, as well as Knee Pain and Knee Injury.
NextEpidemiologyFrequencyUnited StatesMeniscal injuries may be the most common knee injury. The prevalence of acute meniscal tears is 61 cases per 100,000 persons.The overall male-to-female incidence is approximately 2.5:1. The peak incidence of meniscal injury for males is in those aged 31-40 years. For females, the peak incidence is in those aged 11-20 years. In patients older than 65 years, the rate of degenerative meniscal tears is 60%. Surgical procedures of the meniscus are performed on an estimated 850,000 patients each year.[3] InternationalEstimates indicate that at least twice the number of meniscus procedures in the United States are performed worldwide.
PreviousNextFunctional AnatomyThe menisci are 2 semilunar wedges in the knee joint positioned between the tibia and the femur. They are essentially extensions of the tibia that act to deepen the articular surfaces of the otherwise relatively flat tibial plateau to accommodate the relatively round femoral condyles. The superior surfaces are concave and in contact with the femoral condyles; the inferior surfaces are flat and conform to the tibial plateaus. The peripheral, convex borders of the menisci are thick and attach to the joint capsule; the opposite border tapers inward to a thin, free edge centrally. Therefore, menisci have a triangular shape in cross section. Each covers approximately two thirds of the corresponding articular surface of the tibia. The medial and lateral menisci each have distinct, individual anatomic characteristics.[4, 5, 6]
The medial meniscus is semicircular or C-shaped and approximately 3.5 cm in length from anterior to posterior. It is asymmetric with a considerably wider posterior horn than anterior horn. Peripherally, the medial meniscus is continuously attached to the joint capsule, with the middle portion being more firmly attached via connection with fibers of the deep medial collateral ligament. It is anchored to the tibia by the coronary (meniscotibial) ligaments.
The posterior horn of the medial meniscus inserts in the posterior intercondylar fossa directly anterior to the posterior cruciate ligament. The anterior horn attachment is more variable, distributed in a 6- to 8-mm area anterior to the anterior cruciate ligament (ACL) tibial attachment in the anterior intercondylar fossa. Some anterior fibers attach over the anterior periphery of the tibial articular surface, and some posterior fibers of the anterior horn merge with the transverse meniscal ligament that connects to the lateral meniscus.
The lateral meniscus is more nearly circular or O-shaped and covers a larger portion of the tibial plateau surface than the medial meniscus. Its length from anterior to posterior is slightly less than the medial meniscus, and it has an almost uniform width. There is attachment to the joint capsule peripherally, except in the region of the middle one third, where there is no attachment but rather a hiatus for the popliteal tendon.
Unlike the medial meniscus, there is no attachment of the lateral meniscus to the lateral collateral ligament, but the lateral meniscus is anchored to the tibia via coronary (meniscotibial) ligaments. Posteriorly, the lateral meniscus is uniquely attached to the medial femoral condyle by meniscofemoral ligaments. These ligaments are highly variable and pass anterior (ligament of Humphrey) and/or posterior (ligament of Wrisberg) to the posterior cruciate ligament. The posterior attachment to the tibia is just anterior to the medial meniscus attachment in the posterior intercondylar fossa. The anterior horn inserts anterior to the lateral tibial spine and in close proximity to the ACL tibial insertion. Some fibers actually may blend into the ACL.
Despite their attachments, both menisci have mobility. The medial meniscus, with excursion of approximately 5 mm, is half as mobile as the lateral meniscus, whose mobility may exceed 10 mm. The anterior horns are more mobile than the posterior horns. This mobility allows for improved conformity of the tibiofemoral joint. Because the posterior horn of the medial meniscus has the least movement, it is at greatest risk for disruption.
The microanatomy of the meniscus is dense fibrocartilage composed of cells and an extracellular matrix of collagen fibers in network. The cells are termed fibrochondrocytes because they appear to be a mixture of fibroblasts and chondrocytes. These cells are responsible for the synthesis and maintenance of the extracellular fibrocartilaginous matrix.
The most abundant component of the menisci is collagen (75%)—mainly type I collagen (>90%) but it also contains types II, III, V, and VI. Collagen fibers are arranged mostly along a longitudinal or circumferential direction, with some interwoven radial and oblique fibers. The circumferential fibers are related directly to the menisci's functional ability to dissipate compressive loads. The other fibers act primarily as ties to enhance structural rigidity and to help prevent longitudinal splitting. The extracellular matrix also includes proteoglycans, glycoproteins, and elastin.
Most meniscal tissue is avascular and depends on passive diffusion and mechanical pumping to provide nutrition to the fibrocytes within the meniscal substance. Arnoczky and Warren demonstrated the important vascular anatomy of the menisci.[7, 8] The limited peripheral blood supply originates from the medial and lateral inferior and superior geniculate arteries. Branches from these vessels give rise to a perimeniscal capillary plexus within the synovium and joint capsule, which, in turn, supplies the meniscus periphery.
Studies have shown that 10-30% of the periphery of the medial meniscus and 10-25% of the lateral meniscus receives a vascular supply; the remainder receives its nutrition from the synovial fluid from passive diffusion and mechanical pumping. A few terminal branches of these vessels, along with the middle geniculate artery through the synovial covering of the anterior and posterior horn attachments, supply increased vascularity to the meniscal horns. The potential for vascular ingrowth is essential for successful meniscal healing and surgical repair. Various zones of the meniscus are described based on the blood supply; the red zone is the well-vascularized periphery, the red-white zone is the middle portion with vascularity peripherally but not centrally, and the white zone is the central avascular portion.
The neuroanatomy of the meniscus is not well described. However, the distribution of neural elements has been demonstrated in essentially the same anatomic distribution as the vascular supply. The anterior and posterior horns are the most richly innervated, and the body innervation follows the pattern along the periphery. Although not entirely clear, these nerve endings are believed to play a role in sensory feedback and proprioception. The greater innervation of the horns of the meniscus reflects the need for feedback at the extremes of flexion and extension, when the meniscal horns are compressed and neural elements are activated.[4, 5, 6]
The meniscus has unique anatomic properties. An understanding of this anatomy is essential to comprehending its important functions, which include load bearing, load and force distribution, joint stability, joint lubrication, and proprioception.[4, 5, 9] One of the primary functions is to provide load bearing across the knee joint. Fifty percent of the compressive load in the knee is transferred by the menisci in extension, whereas up to 85% of the load is transferred at 90° of flexion. The collagen orientation makes this load bearing possible by converting the compressive forces to tensile forces.
Load and forces are distributed across a much larger surface area because of the menisci, which (1) decrease focal contact pressure by increasing the contact area and (2) protect the underlying articular cartilage. Resection of 15-34% of a meniscus may increase contact pressure by more than 350%. Normal knees have 20% better shock-absorbing capacity than meniscectomized knees.
Joint stability is increased because of meniscal structure, which allows increased congruence and conformity between the femoral condyles and tibial plateaus.[4, 5] The wedge-shaped meniscus attached to the tibia serves as a secondary stabilizer. For example, the posterior horn acts as a shim to resist anterior tibial translation relative to the femur. Meniscectomy alone may not increase knee laxity, but it has been shown that in association with ACL deficiency, anterior laxity is increased. Meniscal lubrication occurs by fluid exudation across the surface, much like articular cartilage.
The classification of meniscal tears provides a description of pathoanatomy. The types of meniscus tears are (1) longitudinal tears that may take the shape of a bucket handle if displaced, (2) radial tears, (3) parrot-beak or oblique flap tears, (4) horizontal tears, and (5) complex tears that combine variants of the above.
PreviousProceed to Clinical Presentation , Meniscus Injuries






0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.