![]()
Overview
Competitive and recreational sporting opportunities for patients with disabilities have increased tremendously. One particular group of patients that has benefited from these opportunities and now participates in sports in ever-enlarging numbers is individuals with paraplegia. For the purposes of this article, paraplegia is defined as complete or incomplete paralysis in the lower extremities such that a wheelchair must be used as the primary mode of mobility. (See also the articles Spinal Cord Injury: Definition, Epidemiology, Pathophysiology in the Physical Medicine and Rehabilitation section of this site, and Spinal Cord Injuries in the Emergency Medicine section.)
The number of people with paraplegia continues to increase over time as general health and life expectancy has been increased to levels that are comparable to individuals without paraplegia. As a result, the demand by those with paraplegia for competitive and recreational sporting opportunities has exploded. An additional factor for the rapid growth of participation in sporting activities by those with paraplegia is the improvement in accessibility, as well as the improved designs of sporting facilities and wheelchairs, which allow for meaningful athletic competition.
Sports participation is an indispensable method of modern rehabilitation. Especially after medical rehabilitation is completed, sports have an invaluable therapeutic value in renewing the paraplegic's lost powers, helping coordination, and maintaining stamina. Today, individuals with paraplegia participate in all types of sports for competition, enjoyment, and to improve overall fitness.
NextHistory
The demand for competitive wheelchair sports traces its roots back to World War II.[1, 2] Thousands of young veterans returned from the war with physical disabilities; however, the desire to pursue sports was undiminished by these veterans' disabilities. Organized wheelchair sports began with wheelchair basketball. Teams were first formed in Veterans Administration hospitals and then expanded with community-based teams throughout the United States. Today, an extensive professional league, the National Wheelchair Basketball Association (NWBA), continues this tradition.[1] Amateur and professional leagues have formed in other team sports (eg, rugby) and in individual sports (eg, tennis, skiing, track and field).
Olympic-style games for athletes with disabilities were organized for the first time in Rome in 1960.[3] Now called the Paralympics, these games occur every 4 years for persons who fall within 1 of 6 disability groups, including spinal cord injury (SCI). A 2-week event that occurs after the regular Olympics, the Paralympics is run by the International Paralympics Committee (IPC) and has grown into an elite event that attracts nearly 4000 disabled athletes from 136 countries throughout the world.[3]
Overall, the benefits for persons with paraplegia or even tetraplegia to participate in sports activities is as varied as it is significant. Muraki and co-authors "demonstrated that sports activity can improve the psychological status, irrespective of tetraplegics and paraplegics, and that the psychological benefits are emphasized by sports activity at high frequency."[4]
PreviousNextCommonly Participated Sports
Almost any sport in which able-bodied athletes can participate in can be modified to fit participation by individuals with paraplegia. Such common sports include aerobics, air-guns, archery, basketball, bicycling/hand cycling, bowling, canoeing, fishing, football, golf, horseback riding, kayaking, soccer, quad rugby, racquetball, distance racing, rowing, sailing, road racing, skiing, sled hockey, softball, swimming, table tennis, tennis, track and field, trap/skeet shooting, water skiing, weight lifting, wheelchair fencing, and water polo.
PreviousNextSpecific Examples of More Popular SportsWheelchair basketball
The oldest team wheelchair sport is also one of the most physically demanding and one of the most popular. The NWBA nationally organizes wheelchair basketball competitions among 180 teams, which make up 21 conferences. Annual national tournaments are held for male and female divisions, junior divisions, and intercollegiate divisions.[1] The rules are modified from the National Collegiate Athletic Association rules. New wheelchair modifications continue to make the sport more competitive and even fan friendly.
Long-distance cycling/marathons
Fueled by continued technical improvements, road racing has become the most popular form of recreational and competitive activity for individuals with paraplegia. A wheelchair division now exists at almost every major marathon after the first disabled athlete competed at the Boston Marathon in 1975. The participants' racing times continue to improve and amaze. Sports 'n Spokes magazine is a publication that is dedicated to this activity and annually compiles a list of handcycle and bicycle manufacturers.
Quad rugby
Always a hit with new spectators at national wheelchair competitions, rugby is a unique sport for individuals with tetraplegia. The game is played on a basketball court by 4-member teams using a volleyball. Players are classified according to the US Quad Rugby Association (USQRA) classification system. Each class has a point value, and teams are balanced by limiting the number of points on any team to 8. The object is to carry the ball across the other team's goal line. Although the game does not really share similar rules to typical rugby, quad rugby does share a similar spirit and competitiveness. Quad rugby games can also lead to a fair amount of injuries, and the SCI physician can become quite busy during the competition.
Wheelchair tennis
First organized by the National Foundation of Wheelchair Tennis (NFWT) in 1980, the sport of wheelchair tennis is now under the aegis of the US Tennis Association (USTA). The sport follows the rules of the USTA; however, the player in a wheelchair is allowed 2 bounces instead of 1. The professional wheelchair tennis circuit is one of the few wheelchair sports that is largely independent of classification. Although this has increased the popularity of the sport among spectators without SCI, it has limited the success of players with higher-level paraplegia. On a recreational level, wheelchair tennis is one of the few sports where persons with SCI can compete with their able-bodied friends and family members.
Skiing
Also fueled by technologic revolutions, recreational and competitive skiing is extremely popular among those with SCI injuries. Persons with paraplegia and quadriplegia can ski using a sit-ski, mono-ski, or bi-ski. Numerous camps and opportunities for novices to learn and enjoy the sport are available.
Sailing
Another sporting activity that has been made increasingly accessible by continued advances in adaptive equipment is sailing. This activity offers persons with disabilities a feeling of freedom that is unmatched in almost any other sport. The National Ocean Access Project (NOAP) is a leading organization that promotes sailing for people with disabilities. The Shake-A-Leg program in Miami, Florida, operates with the support of the Miami Project to Cure Paralysis, and attracts sailors with disabilities from all over the world to test the latest equipment and train for international sailing competitions.
Fencing
Fencing can be accomplished if the wheelchair is specially modified. A fencing sports wheelchair includes a seat that is mounted to a base. A pedestal underlies the base such that the base is selectively rotatable. There is also a platform that has an upper surface to which the pedestal is affixed, as well as a lower surface. At least 3 wheels are mounted to the platform so that the wheels extend beneath the lower surface of the platform. In addition, there is a lever means for converting single-handed manual motion into forward and backward translation of the platform.
Disabled motorsports
Disabled motorsports include any motorsport that is accessible to the disabled or to wheelchair users, such as those that use motorbikes, quad bikes, go carts, etc. In fact, persons with SCI can participate in anything with an engine.
Other popular wheelchair activities:Water PoloDivingExtreme sports UK four-cross downhill mountain bikingExtreme wheelchair racing and jumping TankChair – An off-road wheelchair that is used for extreme wheelchair sportsParalympic sports
The Paralympics includes 27 sports (20 Paralympic summer sports, 5 Paralympic winter sports, 2 non-Paralympic sports) as follows[3] :
Alpine skiingArcheryAthleticsBiathlonBocciaBowls (non-Paralympic)Cross-country skiingCyclingEquestrianFootball 5-a-SideFootball 7-a-SideGoalballIce sledge hockeyJudoPower liftingRowingSailingShootingSwimmingTable tennisVolleyball (sitting)Wheelchair basketballWheelchair curlingWheelchair dance sport (non-Paralympic)Wheelchair fencingWheelchair rugbyWheelchair tennisPreviousNextParalympics
In 1948, Sir Ludwig Guttmann at the National Spinal Injuries Unit at Stoke Mandeville Hospital in Buckinghamshire, England, introduced the first Stoke Mandeville Games for World War II veterans with SCI.[2, 3] Later, other organizations were formed and sponsored competitions for persons with disabilities. As time went by, multidisability competitions developed and eventually grew into the Paralympics, or "Parallel Games for Athletes with Disabilities."[2]
After 1960, attempts were made to hold every fourth Paralympics in the Olympic host city and were successful in 1960 at Rome and 1964 in Tokyo. However, until 1988, subsequent host cities refused to host the competitions.[2] As the popularity of the Paralympics grew, the IPC was formed to coordinate the Paralympic games and other multidisability competitions on the elite sports level. In 1976, the scope of the Games was widened to accept other disabilities.[2, 3] The Paralympics games have been operating under the IPC since 1994 in Bonn, Germany. In 2000, the summer Paralympics in Sydney consisted of over 4000 athletes from 125 nations competing in 19 events (plus track and field) in both individual and team sports. For the 2004 games in Athens, over 3800 athletes from 136 nations participated.
As with any event of this size, the Paralympics faces significant challenges as it heads into the future. Many of the issues are similar to those found in the regular Olympics, including the use of performance-enhancing substances. The policy of the IPC is that the playing field should be level; unfortunately, 7 Paralympic athletes in the 2004 Athens games were sanctioned for the use of performance-enhancing agents. As a result, the IPC developed the IPC Anti-doping Code in the spirit of fair play to prevent doping in sports for athletes with a disability and in conformity with the general principles developed by the World Anti-doping Agency (WADA), the World Anti-doping Code (WADC).[3]
Another challenge is development; that is, money needs to be raised to keep the Paralympics program going. In November 2004 at the IPC Development Conference, the Paralympic Movement agreed on 5 core areas for development: athlete development, leadership development, organizational development, knowledge development, and global Paralympic development.[3]
Despite these challenges, however, there has been keen excitement regarding the 2012 Paralympic games in London, England. The list of sports and qualification guide is listed at www.paralympic.org.
PreviousNextClassification
An individual who cannot participate or compete in a sport on reasonably equal terms with persons without disabilities because of a functional disadvantage due to permanent disability is eligible for participation in that sport within the IPC program. The classification of athletes was created to equal the playing field within sporting activities in which athletes with disabilities participate. In addition to the classification systems that exist for each injury type (eg, amputation, SCI), unique classification systems exist for each sport. An athlete may be eligible for one sport and not another.
Athletes with SCI have obvious unique functional concerns. The classification of athletes with SCI, while imperfect, tries to take these concerns into account. Athletes in the Paralympics traditionally belong to 1 of 6 different disability groups, divided based on the level of the injury: amputees, persons with cerebral palsy, persons with visual impairment, persons with SCIs, persons with intellectual disability, and a group that includes individuals who do not fit into the aforementioned groups.[5] The first class, for those with cervical injury is subdivided into 3 more classes (A, B, and C) based on upper extremity strength.
The need to change functional classes is consistently reviewed. When an athlete starts competing, he or she is allocated a class that may be reviewed throughout the athlete's career. Individuals are certified in each sport to conduct the process of classification, and these officials are known as classifiers.
Certain sports rate players individually, regardless of diagnosis. For example, wheelchair basketball has a unique system; the 8 different classifications are based on sport-specific tests of shooting, passing, rebounding, pushing, and dribbling abilities, rather than a medical diagnosis or muscle function examination. Higher classification numbers represent greater basketball skills. Athletes are given a numeric point value based on their classification status; the maximum allowable points on the floor is 14.0.
In 2003, the IPC developed a classification strategy with the overall objective to support and coordinate the ongoing development of accurate, reliable, consistent, and credible sport-focused classification systems and their implementation. The IPC Classification Code Version 1.0 is a direct result of recommendations made in this strategy. The results and classification code was published in 2007 and can be found at http://www.paralympic.org/sites/default/files/document/ 120201084329386_2008_2_Classification_Code6.pdf.
The Code is complemented by International Standards that provide the technical and operational requirements for classification. The Code applies to all sports within the Paralympic Movement. Adherence to the International Standards is mandatory for compliance with the Code. The 3 International Standards are as follows:
Athlete evaluation – Procedures for the assessment of athletes and the allocation of sport classProtests and appealsClassifier training and certification
In 2011 the IPC published updated guidelines in skiing. They can be found at http://ipc-alpineskiing.org/Classification/, with 12 classification levels.
Finally, the IPC recently adopted the research paper on “IPC Position Stand – Background and Scientific Rationale for Classification in Paralympic Sport†from Tweedy and Vanlandewijck.[6]
PreviousNextMedical Benefits of Exercise
Multiple studies have found both physical and psychologic benefits from exercise in persons with SCI and that training programs for persons with disabilities can increase maximum oxygen consumption, decrease heart rate at a given work load, increase grip strength, increase arm work capacity, and increase general well-being. However, the amount of studies actually examining these issues is few, and further studies are needed. Please review some of the recent references listed in the References section.
Cardiovascular risk factors
One study showed significant association between cardiovascular risk factors and fitness, similar to that observed in persons without paraplegia.[7] Arm ergometry exercise reduced serum lipids and improved cholesterol ratios as peak oxygen consumption increased. Another study suggested that further benefit to the cholesterol profile was attained if exercise intensity achieved 70-80% of the heart rate reserve.[8]
Strength measures
Common sense would dictate that strength training increases strength and endurance. However, the extent of benefits from a coordinated anaerobic program was not definitively demonstrated until Nash et al published their findings that circuit resistance training over 4 months improved the muscle strength, endurance, and anaerobic power of middle-aged men with paraplegia while significantly reducing their shoulder pain.[9]
Cardiovascular measures
In a 1975 report, Zwiren and Ba-Or demonstrated that athletes in wheelchairs had significantly higher peak oxygen uptake than sedentary individuals in wheelchairs or sedentary individuals without SCI when performing arm exercises.[10] A 1988 study by Davis and Shephard demonstrated that highly active persons with paraplegia showed significantly better cardiovascular responses in multiple measures on cardiac function than inactive persons with paraplegia.[11]
De Groot found improvements in lipid profile, insulin resistance, and other cardiovascular parameters in patients with paraplegia who engaged in exercise.[12]
Psychosocial benefits
Persons with SCI have similar psychosocial ailments as those in persons without SCI but in larger numbers. Depression and feelings of isolation are common. Limited studies have found that exercise in persons with disabilities has led to increased feelings of well-being.[4, 13] Sports and regular activities can also encourage new friendships and help patients develop social support networks. Another study suggested that athletes in wheelchairs are more adventuresome and tough minded than inactive peers. However, whether some of these individuals participated in sports before the injury because they were more tough minded is unclear. In summary, athletes with disabilities seem to gain similar psychologic benefits from sports and exercise as athletes without SCI.
PreviousNextSpecial Medical Risks Associated With Exercise in Individuals With ParaplegiaEpidemiology
It is not entirely clear how many athletes with paraplegia become injured playing sport. One study[14] showed that 24% of all athletes participating in the 2010 Winter Paralympic Games suffered injury. The injury risk was significantly higher than during the 2002 (9.4%) and 2006 (8.4%) Winter Paralympic Games. The authors speculated this increase may have reflected improved data collection systems, but also highlighted a high risk of acute injury in alpine skiing and ice sledge hockey at Paralympic Games.
Specific injury types are discussed below.
Cardiovascular risks
Individuals with paraplegia are reported to have higher resting heart rates and lower stroke volumes while at rest and during exercise than able-bodied individuals. Additionally, persons with thoracic paraplegia have higher resting and exercise catecholamine levels than persons without SCI and persons with cervical SCI. As a result, paraplegic patients reportedly have a degree of excess cardiovascular strain, because a greater percentage of heart rate reserve is required to satisfy a given work level. Whether this translates into any risk of cardiovascular injury is uncertain.
Shoulder and musculoskeletal injuries
Persons with paraplegia depend upon the upper extremities for mobility and transfer. As a result, upper-extremity pain is the most common reported physical injury in persons with SCI, and the shoulder is commonly the most painful joint because it is often the end-bearer of weight and is subjected to significant repetitive strain. Rotator cuff tendinitis, frank tears, and general impingement syndrome are the most common shoulder injuries. Many practitioners believe shoulder pain is worsened in persons with paraplegia by muscle imbalances because overly strong anterior chest and arm muscles overpower the weak posterior scapular and cervical stabilizers. Training programs that emphasize strengthening these weak stabilizers and stretching tight anterior muscles have been proposed to reduce shoulder pain and to improve athletic performance. Other upper-extremity problems include carpal tunnel syndrome, wrist tendinitis, and elbow pain.
Autonomic hyperreflexia
Often observed when persons with SCI are exercising under the control of an electrical current, autonomic hyperreflexia (AH) is most dangerous when it goes unrecognized. Usually limited to persons with SCI above the T6 level, AH occurs because the dissociated sympathetic nervous system becomes activated and is not subject to inhibitory mechanisms. Sympathetic activity is usually initiated by an offending stimulus (eg, kinked Foley catheter). If the offending stimulus is not found, blood pressure can elevate to malignant, life-threatening levels. Some racers in wheelchairs actually induce AH as an ergonomic aid for racing, but this practice is discouraged by physicians.
Fractures
Most athletes with SCIs develop lower-extremity osteoporosis as a result of disuse, immobility, and other factors; these individuals are at higher risk for lower-extremity long-bone (eg, femur, tibia) fractures after simple falls and minor injuries. Aggressive team sports (eg, rugby, basketball) create special risks for fracture injuries. Most lower-extremity fractures in patients with paraplegia have historically been treated nonoperatively; however, in wheelchair athletes, this policy needs to be revisited because operative care might lead to a quicker return to the playing field, with better outcomes and sports achievement.
Overuse injuries
Quite common among athletes with paraplegia, such overuse can cause chronic pain syndromes. These include upper extremities tendonitis, bursitis, and skin maceration and breakdown. Cross-training, proper equipment, and proper training are all elements that lead to preventing these injuries or limiting them to some degree.
PreviousNextSpecial Topics
Wheelchair athletes require specific wheelchairs that allow for maximum function or speed. Typical measurements or design requirements that are established for the sports wheelchair include:
Removable anti-tippersAdjustable tension backrest24" wheelsAdjustable seat dumpVariable camber4" castersFore-aft axle positionRemovable bumpersHeight-adjustable footrest4 wheelsSingle anti-tipper (pivot)16" seat width and backrest heightNylon upholstery
Interestingly, Authier and co-authors published a method of sports wheelchair fabrication that costs less than USD $125 without the wheels.[15] It is these authors' hope that the publication of their design will lead to the spread of sports wheelchairs for the poor in less-developed nations.
Previous, Sports Participation by Paraplegics
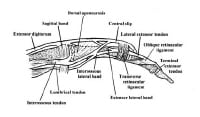 Lateral view of relevant finger anatomy.
Lateral view of relevant finger anatomy. 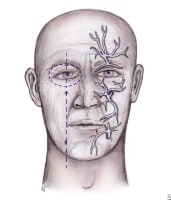 Distribution of nerves for regional anesthesia of the face.
Distribution of nerves for regional anesthesia of the face.  Top: Improper repair of an angled laceration. Bottom: Proper repair of an angled laceration, with creation of perpendicular edges for a flush repair. Repair
Top: Improper repair of an angled laceration. Bottom: Proper repair of an angled laceration, with creation of perpendicular edges for a flush repair. Repair Steps to repair lip laceration. A 3-layered approach is needed, as depicted.
Steps to repair lip laceration. A 3-layered approach is needed, as depicted.  MRI displaying a ruptured anterior cruciate ligament.
MRI displaying a ruptured anterior cruciate ligament. 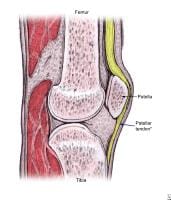 The proximal patellar tendon is most commonly affected in jumper's knee.
The proximal patellar tendon is most commonly affected in jumper's knee. 





