Practice Essentials
Osteitis pubis is an inflammation of the pubic symphysis and surrounding muscle insertions. First described in patients who underwent suprapubic surgery, it remains a well-known complication of invasive procedures about the pelvis. It may also occur as an inflammatory process in athletes.
Signs and symptomsThe presenting symptoms of osteitis pubis can be almost any complaint about the groin or lower abdomen. Common complaints include the following:
Pain localized over the symphysis and radiating outwardAdductor pain or lower abdominal pain that then localizes to the pubic area (often unilaterally)Pain exacerbated by activities such as running, pivoting on 1 leg, kicking, or pushing off to change direction, as well as by lying on the side Pain occurring with walking, climbing stairs, coughing, or sneezingA sensation of clicking or popping upon rising from a seated position, turning over in bed, or walking on uneven groundWeakness and difficulty ambulatingFever, chills, or rigors along with pubic pain (osteomyelitis must be ruled out)Physical findings for osteitis pubis can vary greatly.[1] Such findings may include the following:
Tenderness to palpation in the area over the superior pubic ramusWhen sacral innominate dysfunction is a cause, pain over one or both sacroiliac (SI) joints, often in conjunction with piriformis spasm and resultant sciatic-type pain With discrepancies of leg length (anatomic or functional), hip pain in the longer limbThe most specific test for osteitis pubis is a direct-pressure spring test, performed as follows:
Palpate the athlete’s pubic bone directly over the pubic symphysis; tenderness to touch is often noted at that pointSlide your fingertips a few centimeters laterally to each side, and apply direct pressure on the pubic rami; with this pressure, the patient feels pain in the symphysis To see if one side or the other produces more pain or lateral pain, apply ipsilateral pressureThe examination may also include the following as appropriate:
Checking for inguinal herniaAssessment of muscle weakness, especially in hip adductors or flexorsGait assessment Gynecologic examination, if other symptoms suggest possible pelvic inflammatory disease (PID)Rectal examination, if symptoms suggest possible prostatitisDiagnosisLaboratory studies are not required to make the diagnosis, but some may be helpful in eliminating other causes, including the following:
Complete blood count (CBC)Erythrocyte sedimentation rate (ESR)UrinalysisIf the patient is febrile, a blood cultureImaging studies that may be helpful include the following:
Plain radiographyBone scanning (technetium-99m)Single-photon emission computed tomography (SPECT)Magnetic resonance imaging (MRI)Computed tomography (CT)Other studies that may be considered are as follows:
Aspiration of the pubic symphysis for culture, when the patient is febrile but blood cultures are negativeHerniography, when a sports hernia is a strong considerationTreatmentRest and time are the primary healing mechanisms. Physical therapy (PT) may be useful during the early stage and has the following goals:
To help alleviate painTo start correcting the mechanical problems that precipitated the injuryElements of therapy may include the following:
Heat or ice may provide symptomatic reliefProgressive ambulation with the aid of an assistive device and possible orthosesAvoidance of any exercise that may place stress on the pelvic ringDynamic stabilization techniquesManipulationUltrasound and electrical stimulationOnce the patient is free of pain, strengthening therapy can begin. Further PT measures may include the following:
Exercises for the hip flexors, hip adductors, lumbar stabilizers, and abdominal musclesHamstring and quadriceps exercisesStretching (daily or more often)Aquatic conditioning (except frog kicking)Stair-stepping machines (as tolerated)Sports-specific activities, with offending motions added lastManipulationPharmacologic therapy may include the following:
Nonsteroidal anti-inflammatory drugs (NSAIDs)Steroids (oral or injected)Prolotherapy with dextrose and lidocaineSurgery is rarely warranted for osteitis pubis and is generally reserved for failure of conservative management. Surgical approaches, if indicated, include the following:
CurettageArthroscopic curettage combined with adductor debridement and reattachmentArthrodesisWedge resectionWide resectionImage library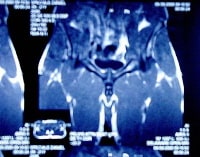 Magnetic resonance image (MRI) from 20-year-old National Hockey League (NHL) player who presented with complaint of pain in testicles, which was worse with skating and with performing off-ice plyometric conditioning. MRI of pelvis combined with history and physical examination indicated diagnosis of osteitis pubis. NextBackground
Magnetic resonance image (MRI) from 20-year-old National Hockey League (NHL) player who presented with complaint of pain in testicles, which was worse with skating and with performing off-ice plyometric conditioning. MRI of pelvis combined with history and physical examination indicated diagnosis of osteitis pubis. NextBackgroundOsteitis pubis is an inflammation of the pubic symphysis and surrounding muscle insertions.[2, 3, 4, 5, 6] It was first described in patients who had undergone suprapubic surgery and remains a well-known complication of invasive procedures about the pelvis. However, it may occur as an inflammatory process in athletes.
Although the exact etiology of osteitis pubis is unknown, it is most likely caused by repetitive microtrauma or shearing forces to the pubic symphysis. Sacroiliac (SI) joint motion has a very large impact on the motion about the pubic symphysis. Batt et al postulated that osteitis pubis is a result of muscle injury to the hip adductors or abdominal musculature, causing muscle spasm, which, in turn, produces increased shearing forces across the pubic symphysis.[3]
Multiple sports-related occurrences of this condition have been reported. For instance, in a study of 502 Australian Football League (AFL) players, 161 of whom had sustained a hip or groin injury during their career with the league, Gabbe et al found that players who had had such an groin injury during their time in elite junior football had a nearly 4 times greater chance of missing games because of osteitis pubis than other players did (as well as a 9.59 times greater chance of missing games because of a hip chondral or labral lesion).[7]
PreviousNextAnatomyThe anatomy around the pelvic girdle is quite complex (see the image below). The pelvis is a ring, and any change in the anatomy or in the forces applied to one area will be compensated for throughout the ring. This simple fact makes it easier to understand why a leg-length discrepancy or SI dysfunction can greatly change the shear forces across the pubic symphysis.
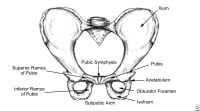 Pelvis, frontal view.
Pelvis, frontal view. In addition, it is important to understand the functions of the muscles that attach to the pubic rami. The hip adductors (ie, the gracilis, adductor longus, adductor brevis, and adductor magnus) originate at the inferior pubic ramus.[8] The pectineus and rectus abdominis muscles, along with the inguinal ligament, insert superiorly. The muscles of the peroneal floor insert posteriorly.
PreviousNextPathophysiologyOsteitis pubis is thought to result from inflammation of the pubis symphysis and is characterized by sclerosis and bony changes of the pubis symphysis (see the image below).[9]
 Radiograph in 19-year-old athlete who presented with 3-week history of groin pull that was not resolving. On clinical examination, pubic spring test reproduced patient's pain, and radiograph was obtained. This image shows classic sclerosis and lysis findings of osteitis pubis around pubic symphysis, with widening of symphysis.
Radiograph in 19-year-old athlete who presented with 3-week history of groin pull that was not resolving. On clinical examination, pubic spring test reproduced patient's pain, and radiograph was obtained. This image shows classic sclerosis and lysis findings of osteitis pubis around pubic symphysis, with widening of symphysis. Osteitis pubis seems to be more prevalent in sports that involve running, kicking, or rapid lateral movements. Sports in which participants develop osteitis pubis more often include the following[2, 4, 5, 8, 10, 11] :
SoccerSprintingIce hockeyAmerican footballSoccer involves a great deal of running and rapid change of direction.[12, 13, 14] These movements can lead to strains of the adductor muscles, which change the forces directed on the pelvis during recovery. Kicking is another inciting motion in soccer. Often, the athlete is not well balanced when planting the foot to kick, and this imbalance places a great deal of strain on the muscles that stabilizing him or her for the kick. This strain translates to abnormal forces across the pubic symphysis.
Sprinting can lead not only to repetitive microtrauma to the pelvis but also to muscle pulls, which are common consequences of the rapid acceleration inherent in sprinting. This condition, coupled with multiple repetitions, can lead to cumulative stress on the pubic symphysis.
Ice hockey has multiple risk factors, including the skating motion and the contact with other players and the dasher boards. Ice hockey players may sustain minor adductor strains, but the continued play and resultant changes in flexibility lead to abnormal forces across the pubic symphysis. This condition can often be aggravated by the rapid changes in direction that are required in ice hockey.
American football also has multiple factors conducive to a high injury rate.[3] The first is the amount of sprinting performed. The second is the frequent violent collisions that often lead to minor injuries, which many athletes may play through. Certain positions (eg, defensive secondary) also demand a great deal of backpedaling, with rapid abduction of one hip to allow the defender to turn and run with a receiver. This motion can lead to hamstring or adductor strains, which change muscle balance and forces applied across the pubic symphysis.
PreviousNextEtiologyThe causes of osteitis pubis are multifactorial. This condition is usually caused by an abnormal shearing force across the pubic symphysis, which, as noted (see above), can itself be caused by muscle imbalance, poor flexibility, and SI joint dysfunction. These abnormalities of pelvic biomechanics—coupled with multiple repetitions of aggravating motions—cause microtrauma to the pubic symphysis, which results in inflammation and muscle spasm.
Conditions associated with osteitis pubis include the following:
Pregnancy and childbirthGynecologic surgeryUrologic surgeryAthletic activities (eg, running, football, soccer, ice hockey, and tennis)[15] Major traumaRepeated minor traumaRheumatologic disordersIn the case of the athlete with a fever and osteomyelitis, Staphylococcus aureus is the most commonly cultured pathogen. Pseudomonas aeruginosa and Escherichia coli have also been reported.
PreviousNextEpidemiologyUnited States statisticsThe exact frequency for osteitis pubis in the United States is difficult to estimate. However, in a study performed by Lloyd-Smith et al in Canada, this condition accounted for 6.3% of the 222 overuse injuries that were studied.[16] In smaller studies, the incidence of osteitis pubis appears to be as much as 5 times more prevalent in males than in females.
International statisticsInternational data are limited. However, there is some reason to think that osteitis pubis may be more common in Europe, because of the popularity of kicking sports such as soccer. A study by Westlin reported that 80% of the athletes who presented to the Sports Medicine Clinic in Malmö, Sweden, had this condition.[17]
Age- and sex-related demographicsAlthough osteitis pubis can affect all age groups, it is rarely encountered in the pediatric population. The disorder occurs most commonly in men aged 30-50 years. Women are more frequently affected in their mid-30s.
The literature suggests that osteitis pubis is more prevalent in men. However, as women continue to lead more active lifestyles and become more involved in sports such as soccer, the relative frequency of this condition in the 2 sexes may change.
PreviousNextPrognosisWith definitive diagnosis and treatment, the prognosis for osteitis pubis is excellent. Although rare instances of mortality from femoral artery involvement have been reported in the obstetric literature, morbidity is more commonly observed secondary to pain and difficulty with ambulation.
In most cases, osteitis pubis resolves with rest. The average time to full recovery is 9.5 months in men and 7.0 months in women. Some reports suggest that recovery may take up to 32 months. Recurrence is more common in males. More aggressive therapy is often needed when an athlete refuses to modify activities or rest.[18] With aggressive physical therapy and judicious use of medications, the athlete often returns to the previous level of activity.
PreviousNextPatient EducationOsteitis pubis is a frustrating condition both for the patient and for the physician; therefore, patient education cannot be overemphasized. Rest is advised. Any activity or exercise that may place stress on the pelvic ring should be avoided. Athletes are advised to refrain from sporting activities for 3-6 months and then to return on a gradual supervised basis.
The most important information to present to athletes and coaches is the importance of incorporating flexibility training into the athlete’s daily routine. In addition, athletes, coaches, and athletic trainers must understand that early identification and treatment of osteitis pubis are crucial.[1] Any groin pull that does not resolve or show marked improvement in 5-7 days should be referred to the team physician. The entire sports medicine team must not only maintain a high index of suspicion but also be thorough in evaluating groin pain.
For patient education resources, see the Men’s Health Center and the Women’s Health Center.
PreviousProceed to Clinical Presentation , Osteitis Pubis






0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.