Practice Essentials
Although clavicle fractures are common and usually heal regardless of the selected treatment, complications are possible, warranting careful attention to these injuries. Multiple attempts have been made to devise a classification scheme for clavicle fractures. The most common system is the following one, created by Allman, in which the clavicle is divided into thirds[1] :
Group I fractures: Middle third injuriesGroup II fractures: Distal third injuriesGroup III fractures: Medial (proximal) third injuriesSigns and symptomsClinical signs and symptoms of clavicle fracture include the following:
The patient may cradle the injured extremity with the uninjured armThe shoulder may appear shortened relative to the opposite side and may droopSwelling, ecchymosis, and tenderness may be noted over the clavicleAbrasion over the clavicle may be noted, suggesting that the fracture was from a direct mechanismCrepitus from the fracture ends rubbing against each other may be noted with gentle manipulationDifficulty breathing or diminished breath sounds on the affected side may indicate a pulmonary injury, such as a pneumothoraxPalpation of the scapula and ribs may reveal a concomitant injuryTenting and blanching of the skin at the fracture site may indicate an impending open fracture, which most often requires surgical stabilization Nonuse of the arm on the affected side is a neonatal presentationAssociated distal nerve dysfunction indicates a brachial plexus injuryDecreased pulses may indicate a subclavian artery injuryVenous stasis, discoloration, and swelling indicate a subclavian venous injury[2, 3]See Clinical Presentation for more detail.
DiagnosisLaboratory studies
Complete blood count (CBC): If a vascular injury is suspected, to check the hemoglobin and hematocrit valuesArterial blood gas (ABG): If a pulmonary injury is suspected or identifiedImaging studies
Chest radiography: Obtain an expiration posteroanterior (PA) chest film (along with the above-mentioned ABG test) if a pulmonary injury is suspected or identified Radiography of the clavicle and shoulderComputed tomography (CT) scanning with 3-dimensional (3-D) reconstruction: To help evaluate displaced fracturesArteriography: If a vascular injury is suspectedUltrasonographySee Workup for more detail.
ManagementThe vast majority of clavicle fractures heal with nonoperative management, which includes the use of a figure-of-eight brace or a simple shoulder sling.
Surgical indications include the following:
Complete fracture displacement[4] Severe displacement causing tenting of the skin with the risk of punctureFractures with 2 cm of shorteningComminuted fractures with a displaced transverse "zed" (or Z-shaped) fragment[4] Neurovascular compromiseDisplaced medial clavicular fractures with mediastinal structures at risk[5] Polytrauma (with multiple fractures): To expedite rehabilitationOpen fracturesAn inability to tolerate closed treatmentFractures with interposed muscleEstablished, symptomatic nonunionConcomitant glenoid neck fracture (floating shoulder)When a midshaft clavicle fracture requires surgical fixation, the commonly performed procedure involves open reduction of the fracture, followed by either insertion of an intramedullary device or fixation with a plate and screws.[6, 7, 8, 9]
In a distal clavicle fracture, stable fixation can be achieved in many ways, including through combinations of a coracoclavicular screw, Dacron or Mersilene tape, tension banding, a Kirschner wire (K-wire), and clavicular plates. Regardless of the exact technique used, the general principles of fracture reduction and fixation and stabilization of the coracoclavicular interval apply.
See Treatment and Medication for more detail.
Image library A posterior view demonstrating a closed clavicle fracture tenting the skin (arrow), which can potentially lead to an open fracture. NextBackground
A posterior view demonstrating a closed clavicle fracture tenting the skin (arrow), which can potentially lead to an open fracture. NextBackgroundClavicle fractures are common and easily recognized because of their subcutaneous position, as shown in the images below. Fracture union usually progresses regardless of the treatment initiated. Despite the innocuous appearance of clavicle fractures, however, potential treatment difficulties and possible complications warrant careful attention to these injuries. (See Prognosis, Treatment, and Medication.)
 A posterior view demonstrating a closed clavicle fracture tenting the skin (arrow), which can potentially lead to an open fracture.
A posterior view demonstrating a closed clavicle fracture tenting the skin (arrow), which can potentially lead to an open fracture. 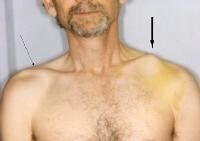 Comparison of both clavicles, with the left tenting the skin (wide arrow).
Comparison of both clavicles, with the left tenting the skin (wide arrow).  Close-up view of clavicle tenting the skin (arrow).
Close-up view of clavicle tenting the skin (arrow). The clavicle is the first bone in the body to ossify, beginning at the fifth week of gestation.[2] Through age 5 years, the growth is primarily through intramembranous ossification. The medial epiphysis ossifies late, beginning at age 12-19 years, and may not completely fuse until age 22-25 years. Physial injuries around this area may be mistaken for fractures, and care should be taken in evaluating injuries. (For patients aged 22-25 years, the Salter-Harris classification for physial injuries can be used, and nonoperative treatment can often be initiated.) (See Anatomy, Clinical Presentation, DDx, and Workup.)
Historically, clavicle fractures have been considered best treated nonoperatively, with good outcomes. Management typically included the use of either a shoulder sling or a figure-of-eight brace. The vast majority of these fractures healed, with variable amounts of cosmetic deformity.
Studies have examined the different patterns of displacement and clinical outcomes of clavicle fractures according to their location. The medical literature has focused predominantly on fractures of the middle and distal clavicle but is still lacking concerning the management of medial clavicle fractures; the literature does, however, indicate that medial clavicle fractures respond well to nonoperative management. Controversy remains concerning operative versus nonoperative treatment of middle and distal clavicle fractures.[10, 11, 12, 13] (See Treatment and Medication.)
Fracture classificationMultiple attempts have been made to devise a classification scheme for clavicle fractures. The most common system is the following one, created by Allman, in which the clavicle is divided into thirds[1] :
Group I fractures: Middle third injuriesGroup II fractures: Distal third injuriesGroup III fractures: Medial (proximal) third injuriesNeer made a significant revision to the Allman classification scheme. Group II (distal clavicle) fractures were further divided into 3 types, based on the location of the clavicle fracture in relation to the coracoclavicular ligaments. The reason for this modification was that distal clavicle fractures behave differently depending on the exact location of the injury. The designations are as follows (see Clinical Presentation and Workup)[14] :
Type I fractures: Minimally displaced and occur lateral to an intact coracoclavicular ligament complex; these fractures may be treated nonoperatively and symptomatically (see the image below) Type II fractures: Occur when the medial fragment is separated from the coracoclavicular ligament complex; the medial fragment is displaced cephalad by the pull of the sternocleidomastoid muscle, and the distal fragment is displaced caudally by the weight of the upper extremity, with the intact coracoclavicular ligament complex; the resulting deformity leads to marked displacement of the fracture ends, predisposing this fracture type to a higher prevalence (up to 30%) of nonunion Type III injuries: Minimally displaced or nondisplaced and extend into the acromioclavicular (AC) joint; as with type I fractures, these injuries can be treated symptomatically; the development of late AC degenerative changes can be treated with distal clavicular excision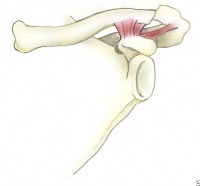 Type I fracture of the distal clavicle (group II). The intact ligaments hold the fragments in place.
Type I fracture of the distal clavicle (group II). The intact ligaments hold the fragments in place. 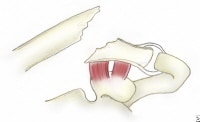 A type II distal clavicle fracture. In type IIA, both conoid and trapezoid ligaments are on the distal segment, while the proximal segment, without ligamentous attachments, is displaced.
A type II distal clavicle fracture. In type IIA, both conoid and trapezoid ligaments are on the distal segment, while the proximal segment, without ligamentous attachments, is displaced.  A type IIB fracture of the distal clavicle. The conoid ligament is ruptured, while the trapezoid ligament remains attached to the distal segment. The proximal fragment is displaced.
A type IIB fracture of the distal clavicle. The conoid ligament is ruptured, while the trapezoid ligament remains attached to the distal segment. The proximal fragment is displaced. The Neer type II fracture was later divided into types IIA and IIB, as follows (see the images below):
Type IIA - Displaced due to fracture medial to the coracoclavicular ligaments; the conoid and trapezoid remain attached to the distal fragment Type IIB - Displaced due to fracture medial to the coracoclavicular ligaments; either the conoid is torn or, more rarely, both the conoid and trapezoid are torn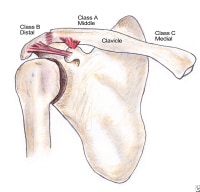 Anatomy of the clavicle indicating potential fracture sites. PreviousNextAnatomy
Anatomy of the clavicle indicating potential fracture sites. PreviousNextAnatomyThe clavicle is an S-shaped bone that acts as a strut between the sternum and the glenohumeral joint. Another function of the clavicle is to help protect the neurovascular bundle that runs behind it. The junction of the middle and distal thirds of the clavicle is a common site of fracture because this is the thinnest part of the bone, and there is relatively little protection by muscular attachments.
Numerous muscular and ligamentous forces act on the clavicle, and knowledge of these differing forces is necessary to understand the nature of displacement of clavicle fractures and why certain fracture patterns tend to cause problems if not reduced and surgically stabilized. (See the image below.)
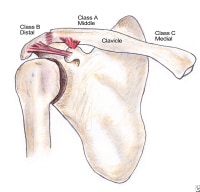 Anatomy of the clavicle indicating potential fracture sites.
Anatomy of the clavicle indicating potential fracture sites. The clavicle articulates with the sternum at the sternoclavicular (SC) joint and with the acromion at the AC joint. Many ligamentous structures attach to the clavicle and provide stability for the articulations with the sternum and the acromion. The primary stabilizers of the SC joint are the anterior and posterior capsules. Other ligamentous structures attaching here are the interclavicular ligament and the costoclavicular ligament. Stability of the SC joint in the anterior-posterior plane is derived predominantly from the posterior capsule, with additional stability conferred by the anterior capsule. The interclavicular and costoclavicular ligaments have little effect on stability of the joint.
At the level of the AC joint, the coracoclavicular and AC ligaments provide stability for the joint. The coracoclavicular ligament is actually 2 separate ligaments, the conoid and the trapezoid, which both attach from the coracoid to the inferior surface of the distal clavicle. Debski et al have delineated the different functions of the conoid and trapezoid in resistance to applied loads to the AC joint.[15] The conoid is the predominant restraint to anterior and superior loading, while the trapezoid is the major restraint to posterior loading at the AC joint. The AC ligament is at the superior-lateral aspect of the clavicle and overlies the AC joint.
Three muscles originate on the clavicle, and 3 muscles insert on it. The muscles that take their origin from the clavicle are as follows:
SternohyoidPectoralis majorDeltoidThe muscles that insert on the clavicle are as follows:
SternocleidomastoidSubclaviusTrapeziusThese 6 muscles may become deforming forces on the clavicle in the presence of a fracture, with the displacement of fracture fragments depending on the location of the fracture in relation to the muscular and ligamentous attachments.
Many other important structures are in extremely close contact with the clavicle and are thus subject to injury in the context of clavicle fractures. The subclavian artery (which becomes the axillary artery as it passes anteriorly to the first rib) and vein are both in close proximity to the middle portion of the clavicle. Additionally, the brachial plexus also passes behind the clavicle posterolateral to the subclavian vessels and is at risk with displaced fractures of the middle clavicle.
The subclavius muscle lies between the clavicle and these neurovascular structures, and, though small, it is believed to prevent more frequent damage to these structures. Reports also exist of injuries to the apices of the lung, most commonly with displaced middle third clavicle fractures.
PreviousNextPathophysiologyBecause of its subcutaneous position, the clavicle may be fractured easily, with the fracture often being an isolated injury. However, clavicle fractures are also common in the context of high-energy injury or multiple traumatic injuries. In these situations, it is important to examine the patient for other associated injuries, such as rib fractures, scapula fractures, other fractures about the shoulder girdle, pulmonary contusion, pneumothorax, hemothorax, and closed head injuries. (See the image below.)
 Clavicle fracture with rib fractures. Remember to look for associated injuries.
Clavicle fracture with rib fractures. Remember to look for associated injuries. The frequency with which the 3 groups of fractures occur is as follows:
Group I (middle third) - Approximately 80%Group II (distal third) - 12-15%Group III (medial third) - Less than 5%Group I fracturesMost group I fractures occur medial to the coracoclavicular ligament, at the junction of the middle and outer third of the clavicle. The proximal fragment is typically displaced upward because of the pull of the sternocleidomastoid muscle. The usual mechanism of injury involves a direct force applied to the lateral aspect of the shoulder as a result of a fall, sporting injury, or motor vehicle accident. Group I fractures are shown in the images below
 Nondisplaced middle clavicle fracture.
Nondisplaced middle clavicle fracture.  Displaced fracture of middle clavicle.
Displaced fracture of middle clavicle.  Displaced middle clavicle fracture. Group II fractures
Displaced middle clavicle fracture. Group II fracturesFractures of the distal third of the clavicle result from a direct blow to the top of the shoulder. They occur distal to the coracoclavicular ligament.[16]
Group III fracturesFractures of the medial third of the clavicle occur as a result of a direct blow to the anterior chest. A diligent search for associated injuries should accompany group III fractures because considerably strong forces are required to fracture this area of the clavicle.
Greenstick or buckle-type fractures are common in children. Most of these fractures are nondisplaced and heal uneventfully.
PreviousNextEtiologyClavicle fractures may be caused by direct or indirect trauma. The most common mechanism is an indirect one, involving a fall directly onto the lateral shoulder.[17, 18, 19] Examples of a direct mechanism would be a blow from a hockey stick or a direct fall onto the clavicle. At-risk athletes include those in football, hockey, and soccer and those at risk for falling during roller skating, skiing, bicycling, or horseback riding.
A less common mechanism for clavicle fractures is a fall onto an outstretched hand (ie, a FOOSH injury). The radiographs below depict clavicle fracture in a hockey player.
 Comminuted fracture in a hockey player. Note the medial fragment tenting the skin.
Comminuted fracture in a hockey player. Note the medial fragment tenting the skin.  Additional view of fracture displacement and comminution in a hockey player. The sternocleidomastoid is the deforming force of the medial fragment.
Additional view of fracture displacement and comminution in a hockey player. The sternocleidomastoid is the deforming force of the medial fragment.  Radiographs after open reduction and internal fixation of a comminuted fracture in a hockey player. PreviousNextEpidemiologyOccurrence in the United States
Radiographs after open reduction and internal fixation of a comminuted fracture in a hockey player. PreviousNextEpidemiologyOccurrence in the United StatesThe clavicle is the most frequently fractured bone in the body in childhood, accounting for 10-16% of all fractures in this age group.
In adults, clavicle fractures account for 2.6-5% of all fractures and 44% of all shoulder girdle injuries.[20, 21, 22] Middle third (group I) fractures account for 69-82% of all fractures of the clavicle, whereas distal third (group II) fractures account for 12%, and medial third (group III) fractures occur in 6% of cases.[20, 21]
Clavicular injuries affect 1 in 1000 people per year. Bimodal incidence occurs in men younger than 25 years and older than 55 years. Pneumothorax occurs in 3% of patients.
International occurrenceThe annual incidence rate of clavicular fractures is estimated to be between 30 and 60 cases per 100,000 population.[12]
Sex- and age-related demographicsClavicular injuries occur 2.5 times more commonly in males than in females, reflecting a greater involvement of males in contact and violent sports and motor vehicle accidents (MVAs).
Clavicle fractures, the most common of all pediatric fractures, can present even in the newborn period, especially following a difficult delivery. A large peak incidence occurs in males younger than 30 years due to sports injuries. A smaller peak occurs in elderly patients, who tend to sustain clavicle fractures (in association with osteoporosis) during low-energy falls.[12]
PreviousNextPrognosisMost clavicle fractures treated nonoperatively heal, although with variable amounts of cosmetic deformity. Younger children generally require shorter periods of immobilization (2-4 wk) than do adolescents and adults (4-8 wk).
ComplicationsNonunion
Nonunion is a failure to show clinical or radiographic progression of healing after 4-6 months. The following are risk factors for nonunion:
Fracture comminutionSignificant fracture displacement or shorteningType 2 fractures of the distal third of the clavicleRefractureFemale sexAdvanced ageFractures with more than 2 cm of shorteningThe nonunion rate for all midclavicle fractures treated nonoperatively is 6%; the rate is 15% for displaced midclavicle fractures treated nonoperatively.[23] Symptoms of nonunion can be pain, motion, or loss of function. Note, however, that many nonunions are asymptomatic and require no treatment. Refer patients with symptomatic nonunion to an orthopedic surgeon to discuss surgical options. In some situations, a bone stimulator to help promote bone healing can be tried before surgery.
Murray et al reported that smoking was the greatest risk factor for nonunion among patients treated nonoperatively for diaphysial clavicle fractures. In a study, the investigators followed the healing course of 941 patients with such fractures and, using multivariate analysis, found that, along with smoking, both comminution and fracture displacement were particularly significant factors in nonunion.
The investigators determined that by using known risk factors, a statistical model can be used to estimate the probability of nonunion in a specific patient and can therefore help to determine whether he or she should be treated surgically. The investigators also concluded that smoking cessation needs to be included in the treatment of diaphysial clavicle fractures.[24]
Malunion
Malunion is when the fracture heals with significant angulation, shortening, and a poor appearance. Mild malunion is common after clavicle fractures, but it is usually not clinically significant. Occasionally, the patient can have pain or a mild limitation in motion or strength. Symptoms from nerve impingement may occur but are uncommon. Surgeries for malunion attempt to restore the clavicular length and correct any angular deformity of the clavicle.
Neurovascular injuries
Group I fractures (middle third of the clavicle) have been associated with injuries to the neurovascular bundle and the pleural dome.
Neurovascular compromise can develop from exuberant callus formation or from malunion. The medial cord and ulnar nerve are affected most often; treatment is surgical in nature. Brachial plexus compression resulting from hypertrophic callus formation may cause peripheral neuropathy.
Intrathoracic injuries
These include the following:
PneumothoraxSubclavian artery and vein injuryInternal jugular vein injuryAxillary artery injuryOther
A spike of bone can form subcutaneously after angulated fractures heal. This can be symptomatic for athletes who wear shoulder pads or for backpackers. If a donut pad is not sufficient to relieve symptoms, surgical excision can be considered. Posttraumatic arthritis can develop if a clavicle fracture enters the AC or SC joints.
Complications after group III fractures (medial third of the clavicle) resemble those associated with posterior sternoclavicular dislocations, including pneumothorax and compression or laceration of the great vessels, trachea, or esophagus.
MortalityWhile the overwhelming majority of clavicle fractures are benign, there is a possibility of associated, life-threatening intrathoracic injuries.
Kendall et al reported a fatality from an isolated clavicle fracture from transection of the subclavian artery,[25] the first such report in the literature. The fatality may have been due to the fact that the fall was not witnessed and the patient lay unassisted for an unknown period of time. The patient never regained spontaneous circulation, and the injury to the subclavian artery was diagnosed at autopsy. The postmortem examination revealed a midclavicular fracture with transection of the subclavian artery. A 2.6-L hemothorax and damage to parietal and apical pleura were noted, but no other injuries were present.
Although this case is unique, it does emphasize the need to be aware of the potentially catastrophic complications of damage to the vascular structures in close proximity to the clavicle.
PreviousNextPatient EducationAt the initial visit, discuss the following with the patient who has a clavicular injury:
A visible prominence may remain at the fracture site after it heals; this may be more evident in thin individualsFracture nonunion is possible, and surgery may be necessaryRefracture is a possibility if the patient engages in contact sports, particularly if he or she returns to play before the bone healing is solidEducate patients about proper placement and adjustment techniques for a figure-of-eight bandage (clavicle strap) and inform them that paresthesias or edema in the hands or fingers indicate that the strap is too tight and should be removed.
Neonatal clavicle fractureAdvise parents to minimize pressure and movement of the ipsilateral arm during handling of a neonate with a clavicle fracture. The parent may try to pin the shirt sleeve of the affected arm to the front of the child’s shirt to minimize movement.
For patient education information, see the First Aid and Injuries Center, as well as Broken Collarbone (Broken Clavicle) and Shoulder Dislocation.
PreviousProceed to Clinical Presentation , Clavicular Injuries






0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.