Background
Osteochondritis dissecans (OCD), by definition, is a disorder of one or more ossification centers, characterized by sequential degeneration or aseptic necrosis and recalcification. OCD lesions involve both bone and cartilage. These lesions differ from acute traumatic osteochondral fractures; however, they may manifest in a similar fashion. OCD lesions also must be differentiated from meniscal pathology. OCD causes 50% of loose bodies in the knee. The etiology of these lesions is multifactorial, including trauma, ischemia, abnormal ossification centers, genetic predisposition, or some combination of these factors. Little agreement exists among researchers regarding the etiology of OCD.
Images of osteochondritis dissecans of the knee are provided below:
 Anteroposterior and lateral radiographs of medial femoral condyle osteochondritis dissecans.
Anteroposterior and lateral radiographs of medial femoral condyle osteochondritis dissecans.  Anteroposterior radiograph of medial femoral condyle osteochondritis dissecans.
Anteroposterior radiograph of medial femoral condyle osteochondritis dissecans.  Arthroscopic view of medial femoral condyle osteochondritis dissecans, hinged medially. Note the large size and thickness of the fragment.
Arthroscopic view of medial femoral condyle osteochondritis dissecans, hinged medially. Note the large size and thickness of the fragment. 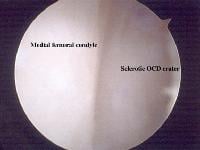 Arthroscopic view of osteochondritis dissecans of the medial femoral condyle. The osteochondral fragment has been elevated from the crater. Note the sclerotic crater with an interposed fibrocartilaginous layer. This lesion has been previously treated with drilling; an old drill hole can be seen faintly at the upper aspect of the crater.
Arthroscopic view of osteochondritis dissecans of the medial femoral condyle. The osteochondral fragment has been elevated from the crater. Note the sclerotic crater with an interposed fibrocartilaginous layer. This lesion has been previously treated with drilling; an old drill hole can be seen faintly at the upper aspect of the crater.  Arthroscopic debridement of the osteochondritis dissecans bed to bleeding bone.
Arthroscopic debridement of the osteochondritis dissecans bed to bleeding bone.  Replacement of the fragment and temporary Kirschner wire stabilization.
Replacement of the fragment and temporary Kirschner wire stabilization.  Completed osteochondritis dissecans stabilization with 2 Herbert screws. On initial examination, the most lateral defect was comminuted and removed; the larger weight-bearing surface was maintained and stabilized.
Completed osteochondritis dissecans stabilization with 2 Herbert screws. On initial examination, the most lateral defect was comminuted and removed; the larger weight-bearing surface was maintained and stabilized. In 1558, Ambroïse Paré removed loose bodies from a knee joint. In 1870, Paget described quiet necrosis within the knee. In 1888, König coined the term "osteochondritis dissecans." He proposed this condition was caused by spontaneous necrosis due to trauma.
With the advent of roentgenography, osteochondrotic conditions in other joints, primarily the hip, were recognized. In 1910, Legg, Calvé, and Perthes independently identified a condition of the hip joint in children, which is now known as Legg-Calvé-Perthes disease. In 1921, Waldenström introduced the term coxa plana (ie, disintegration of capital femoral epiphysis.)
Since the introduction of radiography, 50 additional anatomic sites within the body where OCD can occur have been identified.
Recent studiesTabaddor et al evaluated the efficacy and safety of poly 96L/4D-lactide bioabsorbable copolymer fixation for unstable OCD in 24 adolescents (mean age, 14.4 y). Plain films at an average of 19.2 months after surgery showed interval healing in 9 patients, no significant change in 1, complete healing in 13, and loose bodies with no interval healing in 1. MRIs showed interval healing in 16 of 17 knees at a mean follow-up of 22.4 months.[1]
Pascual-Garrido et al examined the outcomes of surgical procedures for osteochondritis dissecans in 46 adult patients (48 knees), with patients ranging in age from 20 to 49 years. Patients who were treated with surgical cartilage procedures showed durable function and symptomatic improvement at a mean of 4 years follow-up. Patients treated with arthroscopic reduction and internal fixation and loose-body removal had greater improvement in outcome scores than those treated with an osteochondral allograft. Seven knees required revision procedures at a mean follow-up of 14 months.[2]
Adachi et al evaluated the functional and radiographic outcome of retroarticular drilling without bone grafting in 12 patients with juvenile osteochondritis dissecans after 6 months of unsuccessful nonoperative treatment. The mean Lysholm score significantly improved postoperatively (from 72.3 to 95.8). All lesions except 1 healed after retroarticular drilling, and healing was achieved at a mean of 4.4 months on plain radiographs and 7.6 months on magnetic resonance imaging.[3]
Kijowski et al retrospectively compared the sensitivity and specificity of previously described magnetic resonance imaging criteria for the detection of instability in patients with juvenile or adult osteochondritis dissecans of the knee, with arthroscopic findings as the reference standard. Separately, previously described MR imaging criteria for detection of OCD instability were 0-88% sensitive and 21-100% specific for juvenile OCD lesions and 27-54% sensitive and 100% specific for adult OCD lesions. When used together, the criteria were 100% sensitive and 11% specific for instability in juvenile OCD lesions and 100% sensitive and 100% specific for instability in adult OCD lesions. The authors concluded from their findings that previously described MR imaging criteria for OCD instability have high specificity for adult but not juvenile lesions of the knee.[4]
NextEpidemiologyFrequencyUnited StatesThe average age at presentation is 10-20 years, but osteochondritis dissecans may occur in persons of any age group.The male-to-female ratio is 2-3:1.Bilateral involvement is noted in 30-40% of cases.In 85% of cases, lesions are observed on the medial femoral condyle (MFC) of the knee; 15% of cases are observed on the lateral femoral condyle. Of the MFC lesions, 70% occur in the posterolateral aspect. Of patients with OCD, 21-40% have some history of trauma.InternationalIn Sweden, prevalence is reported at the following levels:
In skeletally immature patients, 150 cases per 250,000 people are reported.In skeletally immature female patients, 18 cases per 100,000 people are reported.In skeletally immature male patients, 29 cases per 100,000 people are reported.PreviousNextFunctional AnatomyIn skeletally immature individuals, the vascularity to epiphyseal bone is very good, supporting both osteogenesis and chondrogenesis. With disruption of the epiphyseal vessels, varying degrees and depth of necrosis occur, resulting in a cessation of growth to both osteocytes and chondrocytes. In turn, this pattern leads to nonspecific changes that produce disordered enchondral ossification, resulting in subchondral avascular necrosis or OCD.
Four stages of OCD have been identified, including revascularization and formation of granulation tissue, osteoclasis of necrotic fragments, intertrabecular osteoid deposition, and remodeling of new bone. With delay in the revascularization stage, an osteochondritis dissecans lesion develops. OCD lesions may lead to articular-surface irregularities, which can cause degenerative arthritic changes.
PreviousNextSport Specific BiomechanicsA proposed cause of OCD is an anatomic variation allowing the lateral aspect of the femoral condyle to abut the tibial spine, leading to repetitive localized epiphyseal microtrauma with osteochondral separation and subsequent OCD. This pattern may lead the patient to walk with the tibia externally rotated to avoid this abutment.
PreviousProceed to Clinical Presentation , Knee Osteochondritis Dissecans






0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.